Exploring The Benefits of Home Physiotherapy in Ahmedabad
Embarking on a journey of rehabilitation and recovery, in-home physiotherapy shines as a guiding light, illuminating the path towards optimal healing in the most convenient and comforting way possible. With the option of physiotherapy treatment at home, individuals are granted the invaluable opportunity to receive specialized care within the intimate embrace of their own living spaces. Whether in search of the “best physiotherapy near me” or specifically seeking home physiotherapy in Ahmedabad, the realm of physiotherapy services in Ahmedabad caters to the unique needs and preferences of each individual, fostering a personalized and effective approach to their rehabilitation. By eliminating the need for travel and providing a familiar environment, in-home physiotherapy sets the stage for accelerated progress, allowing individuals to reclaim their physical well-being with greater ease and efficiency.
What are the most important benefits of home physiotherapy in Ahmedabad?
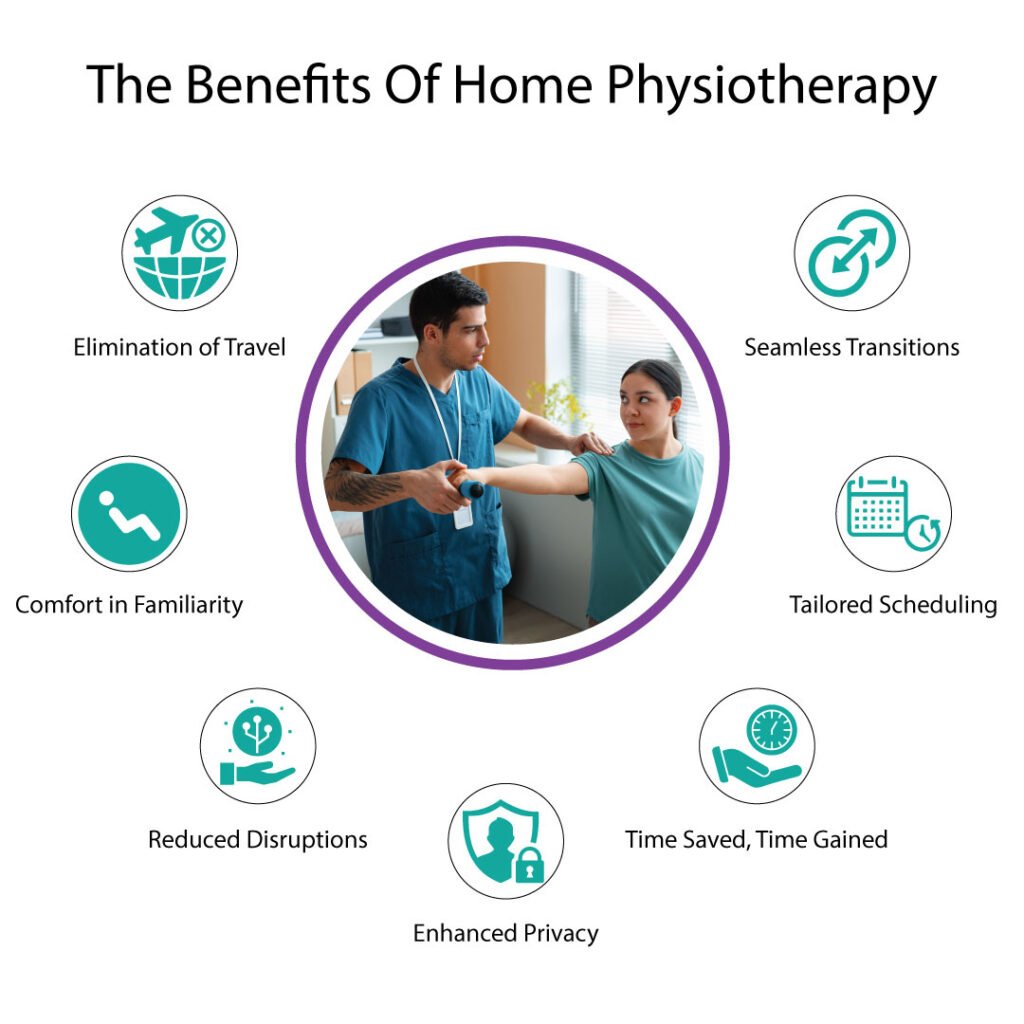
- Elimination of Travel: With in-home physiotherapy, individuals can bid farewell to arduous journeys to clinics or hospitals, sparing themselves the treacherous expedition through unfamiliar streets or the endless waiting at bus stops. They no longer need to search for “best physiotherapy near me” or “physiotherapy services in Ahmedabad,” as the therapeutic oasis is brought right to their doorstep.
- Comfort in Familiarity: In the realm of one’s own abode, a sanctuary of solace, individuals find solace in the known and predictable. Home physiotherapy in Ahmedabad allows patients to embark upon their healing voyage within the cozy confines of their own living quarters. The familiar sights, smells, and sounds provide an unparalleled sense of security, aiding in the augmentation of their therapeutic journey.
- Reduced Disruptions: In-home physiotherapy erases the tormenting prospect of encountering raucous crowds, intrusive noises, and uninvited distractions. Freed from the shackles of external interferences, individuals can immerse themselves fully in their rehabilitation, undisturbed by the cacophonous symphony of a clinical setting.
- Enhanced Privacy: Akin to the secretive dwellings of elusive creatures, one’s home bestows the precious gift of privacy. The in-home setting affords patients the liberty to engage in physiotherapy exercises without prying eyes or judgmental gazes, fostering an atmosphere conducive to vulnerability and personal growth.
- Time Saved, Time Gained: By embracing the realm of in-home physiotherapy, individuals savor the fruits of temporal liberation. The laborious endeavor of traveling to clinics or hospitals is replaced with the opportunity to allocate those precious minutes to other endeavors – be it spending quality time with loved ones, pursuing hobbies, or indulging in much-needed respite.
- Tailored Scheduling: In the realm of home physiotherapy, individuals become the masters of their own temporal domain. They are granted the authority to customize their treatment schedule, ensuring alignment with their personal commitments and obligations. This newfound flexibility injects a sense of empowerment, enabling patients to navigate their rehabilitation journey with increased autonomy.
- Seamless Transitions: The transition from the therapeutic confines of a clinic to the sanctuary of home can be daunting. However, in-home physiotherapy bridges this chasm with seamless grace, fostering continuity of care without abrupt interruptions. The healing process flows uninterrupted, allowing individuals to traverse the path to recovery with unwavering determination.
Advantages of in-home physiotherapy for elders
- Restored Dignity: In the realm of in-home physiotherapy, elderly or disabled individuals find respite from the disheartening ordeal of venturing into unfamiliar territories, which often undermines their sense of dignity. By bringing the therapeutic oasis to their doorstep, home physiotherapy bestows a renewed sense of self-worth, affirming their intrinsic value and honoring their individuality.
- Tailored Accessibility: The aging process or physical disabilities may impose formidable barriers to accessing traditional clinic-based services. However, in-home physiotherapy dismantles these impediments with personalized accessibility solutions. Therapists adeptly navigate the physical constraints of the home environment, employing assistive devices and adaptive techniques to create an inclusive atmosphere that caters to the unique needs of each individual.
- Comforting Familiarity: For elderly or disabled individuals, the journey to a clinic or hospital can be an overwhelming and distressing experience. The haven of home physiotherapy alleviates these anxieties by enveloping patients in the familiar embrace of their own dwelling. The trepidation associated with entering foreign spaces is replaced with a sense of ease, promoting relaxation and allowing individuals to focus wholeheartedly on their rehabilitation.
- Family Engagement: In-home physiotherapy serves as a catalyst for familial involvement in the healing process. Loved ones become active participants, not mere observers, as they bear witness to the transformative power of rehabilitation within the sanctity of their shared home. This collective engagement bolsters emotional support, strengthens familial bonds, and fosters a sense of unity as they work together towards the restoration of physical well-being.
- Holistic Care: The unique demands of elderly or disabled individuals extend beyond physical rehabilitation. In-home physiotherapy acknowledges this reality, embracing a holistic approach that attends to emotional well-being and mental resilience. The intimate home setting provides a safe space for open communication, enabling therapists to address psychosocial aspects and empower individuals to navigate the emotional challenges that often accompany their physical limitations.
- Enhanced Independence: For elderly or disabled individuals, the ability to maintain independence is a cherished aspiration. Home physiotherapy serves as a catalyst for this pursuit, aiming to maximize functional abilities and promote self-sufficiency within the familiar confines of their own abode. Through tailored exercises, adaptive strategies, and progressive goal-setting, individuals are empowered to reclaim their autonomy and regain control over their daily lives.
- Continuity of Care: Transitioning from hospital to home can be a precarious juncture for elderly or disabled individuals. However, in-home physiotherapy ensures a seamless continuum of care, bridging the gap between medical interventions and the comforts of home. By facilitating a smooth transition, individuals experience a consistent and uninterrupted rehabilitative journey, optimizing outcomes and paving the way for lasting improvements in their overall well-being.
- Safe Environment: Safety concerns often loom large for elderly or disabled individuals. In-home physiotherapy mitigates these anxieties by transforming the home environment into a sanctuary of security. Therapists conduct comprehensive assessments, identify potential hazards, and implement appropriate modifications to create a safe space conducive to rehabilitation. This tailored approach minimizes the risk of accidents or falls, instilling confidence and instigating progress in the healing process.
How can home physiotherapy help to reduce the risk of infections?
In the realm of home physiotherapy, individuals can benefit from a reduced risk of exposure to contagious diseases and infections, safeguarding their well-being and fostering a sense of security. By opting for physiotherapy treatment at home, individuals eliminate the need to venture into crowded clinics or hospitals, minimizing their contact with potentially infectious environments. This choice offers a protective cocoon, shielding them from the uncertainties of external spaces and granting peace of mind. Whether searching for “best physiotherapy near me” or specifically seeking home physiotherapy in Ahmedabad, individuals can find solace in the fact that their therapeutic journey transpires within the familiar confines of their own abode, free from the potential hazards of shared waiting areas or treatment facilities. This emphasis on safety, combined with the personalized care provided by physiotherapy services in Ahmedabad, ensures that individuals can pursue their rehabilitation goals without compromising their health or risking exposure to contagious diseases and infections.
Is in-home physiotherapy effective for fast recovery?
In-home physiotherapy plays a pivotal role in facilitating faster and more effective recovery, bringing forth a range of benefits for individuals on their path to wellness. By opting for physiotherapy treatment at home, individuals eliminate the need to travel to clinics or hospitals, saving time and energy that can be redirected towards their rehabilitation. This convenience, coupled with the personalized care provided by physiotherapy services in Ahmedabad, allows for a tailored approach to treatment, addressing individual needs and goals. The familiar environment of home promotes relaxation, enabling patients to feel at ease and focused during their sessions. With reduced disruptions and increased compliance, individuals can engage fully in their treatment plans, leading to enhanced outcomes. Moreover, the continuous monitoring and support offered by home physiotherapy in Ahmedabad ensure that progress is closely tracked, adjustments are made promptly, and recovery milestones are achieved more efficiently. Overall, in-home physiotherapy creates a conducive environment for faster healing, enabling individuals to regain their functional abilities and improve their quality of life.
Conclusion
By bringing physiotherapy treatment directly to one’s home, individuals can access the best physiotherapy near them, including home physiotherapy in Ahmedabad with specialized physiotherapy services in Ahmedabad. This tailored approach to treatment optimizes outcomes, allowing individuals to regain their physical well-being within the familiar embrace of their own living spaces. With the guidance and expertise of Dr. Niraj Patel, renowned as the best physiotherapist in Ahmedabad, individuals embark on a transformative journey towards enhanced mobility, strength, and overall quality of life.